Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.


Shikha Jain, Kriti Khanna, Gautam M Shetty, Sanya Linjhara, Abhay Nene, Disha Ashar & CS Ram
Degenerative lumbar spondylolisthesis (DLS) has been defined as “an acquired anterior displacement of one vertebra over the subjacent vertebra, associated with degenerative changes, without an associated disruption or defect in the vertebral ring” (Matz et al., 2016). Although low back pain is the commonest symptom in patients with DLS, it is frequently associated with leg pain in 42–82% of patients who seek help from orthopedists (Bydon, Alvi, and Goyal, 2019). Leg pain in patients with DLS is a consequence of radicular pain or radiculopathy due to nerve entrapment in the lateral recess or neurogenic claudication due to central canal stenosis, both of which can significantly reduce standing time (ST) and walking time (WT) (Kalichman and Hunter, 2008).
Surgery is often prescribed to patients with radicular pain and/or neurogenic claudication causing significant reduction in ST and WT in patients who have been refractory to conservative treatment (Bydon, Alvi, and Goyal, 2019; Matz et al., 2016). However, non-operative treatment modalities such as physical therapy remain the first-line therapy for patients with DLS (Matz et al., 2016), and previous studies have reported good clinical outcomes with non-operative treatment modalities such as bracing, anti-inflammatory medications and physical therapy in patients with low-grade DLS without neurological deficits (Evans and McCarthy, 2018; Matsunaga, Ijiri, and Hayashi, 2000; Pearson et al., 2008).
Currently, the literature is inconclusive on the effect of a specific physical therapy protocol on specific clinical outcomes such as ST and WT in patients with DLS (Matz et al., 2016). Previous studies investigating the effect of physical therapy have analyzed clinical outcome variables such as neurodeficit, and pain and disability using patient questionnaires such SF-36 (Ware and Sherbourne, 1992), and Oswestry disability index (ODI) (Fairbank and Pynsent, 2000), and did not report improvement in standing time (ST) and walking time (WT) (Matsunaga, Ijiri, and Hayashi, 2000;
Pearson et al., 2008). Hence, the aim of this pilot study was to investigate the effect of a multimodal physical rehabilitation protocol (MPRP) on walking and standing time in patients with DLS and compare it with ST and WT in similar patients who underwent other physiotherapy treatment (OPT) modalities. We hypothesized that MPRP will significantly improve ST and WT in patients with DLS when compared to similar patients who underwent treatment with other PT methods.
This non-randomized, pilot study was conducted prospectively on consecutive patients with unilateral or bilateral leg pain and significant reduction in ST and WT. The study was conducted at two spine rehabilitation clinics (QI Spine Clinic, Dwarka, New Delhi, India and QI Spine Clinic, Gurugram, India) between January 2019 and January 2020.
The inclusion criteria for the study were patients with unilateral or bilateral leg pain with or without back pain due to DLS of any grade as diagnosed on X-ray or magnetic resonance imaging (MRI) done within the last 6 months, reduced ST and WT of <20 minutes, and symptom duration of more than 6 weeks. The exclusion criteria were: “red flag” conditions causing their leg pain (i.e. fever, recent trauma, pain at night or at rest, progressive motor or sensory deficit, saddle anesthesia, unexplained weight loss, and history of cancer); patients having only LBP without leg symptoms due to DLS; epidural injections or spine surgery done previously or during the study period; patients dropping out of treatment; patients with a follow-up of less than 6 months; patients not contactable during follow-up; and patients who did not take any treatment during the study period. Based on the inclusion criteria, patients who joined the multimodal physical rehabilitation treatment program at the study centers after first consultation became part of the MPRP group and patients who refused treatment at out centers became part of the other physiotherapy treatment (OPT) group. The study protocol was approved by an institutional review board and ethics committee. This study was performed in accordance with the Declaration of Helsinki and all participants provided informed consent for participation in the study.
All patients underwent a thorough evaluation including: history (i.e. presenting complaints, past illness, previous surgical or non-surgical treatment, and any reported red flag conditions such as recent trauma, night or at rest pain, fever, unexplained weight loss, progressive motor or sensory deficit, bowel or bladder symptoms, history of cancer, chronic steroid use, and immunosuppression); clinical examination; review of radiographic (X-rays and MRI); and blood reports during the first consultation at the clinic. The severity of spondylolisthesis was graded radiographically using the Meyerding (1932) classification for spondylolisthesis. All patients were clinically examined for posture, lumbar spine range of movement (i.e. forward flexion, extension and lateral flexion), straight leg raising (SLR) test, motor and sensory function (i.e. myotomal and dermatomal loss), deep tendon reflexes (DTR), and evaluated for a directional preference (DP) based on the Mechanical Diagnosis and Therapy (MDT)® system. Directional preference (DP) was defined as a specific repeated end range movement of the lumbar spine that produced centralization, or abolition or decrease of pain symptoms (McKenzie and May, 2003). The DP in a patient was determined by sequentially placing the lumbosacral spine in a series of sustained positions starting with extension, flexion, and flexion-rotation, and recording their effect on back and/ or distal limb pain based on the protocol described by the Mechanical Diagnosis and Therapy (MDT)® system (McKenzie and May, 2003). If distal symptoms in buttock or leg moved back to the midline of spine then this pattern of pain response was termed as “centralization”, whereas if the proximal central back or buttock pain moved distally to the leg (e.g. when pain in the back and buttock, move further down into the calf or foot during testing with repeated end range movements) then this pattern of pain response was termed as “peripheralization” (McKenzie and May, 2003). Once this directional preference was established in a patient, it was prescribed as a treatment intervention to be performed as repeated end range movements at regular intervals as prescribed by the physiotherapist (Table 1).
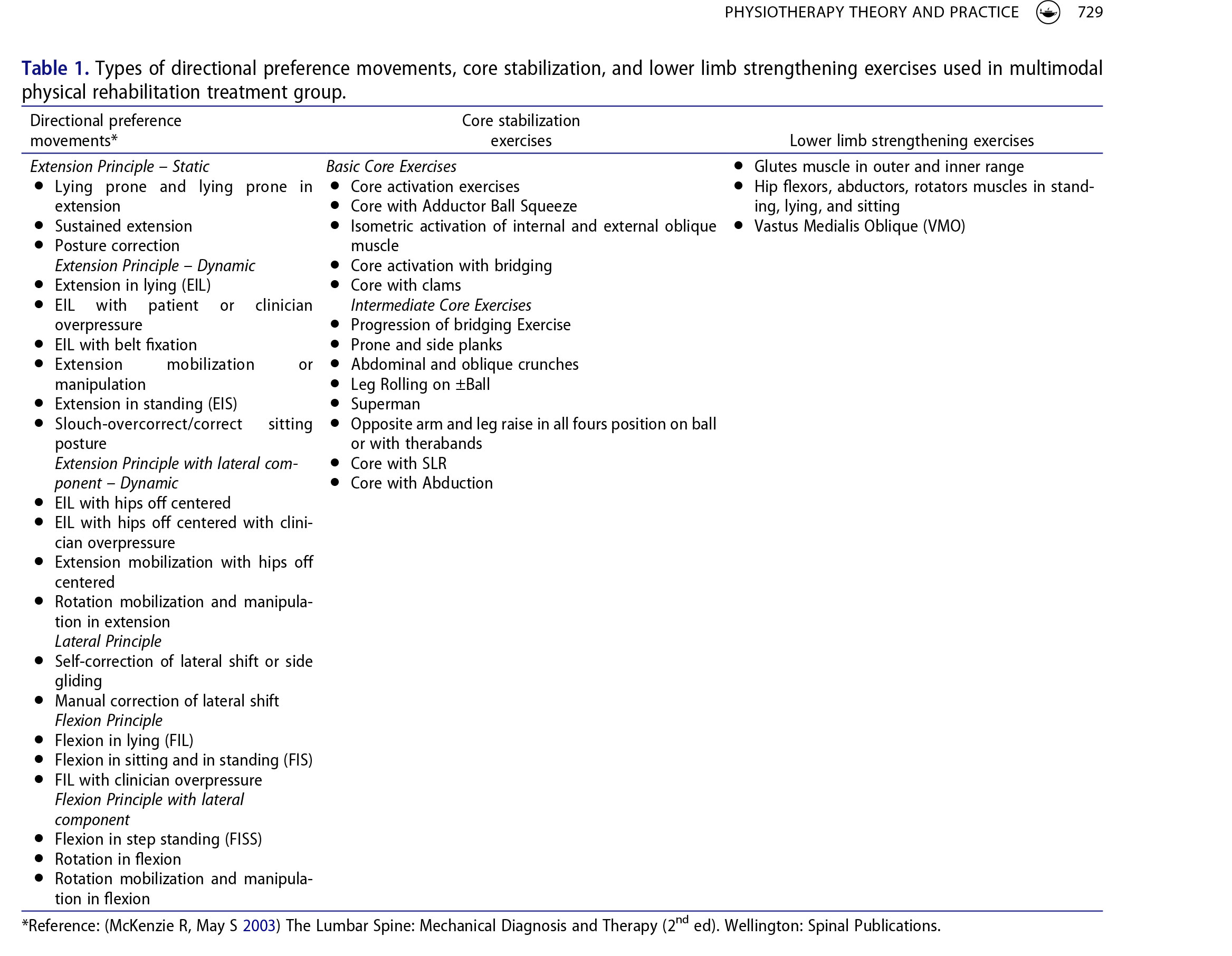
Based on clinical presentation (i.e. bilateral or unilateral pain and/or numbness or paresthesia, positive or negative straight leg raising test, and MRI findings of central canal stenosis, lateral canal or foraminal stenosis with nerve compression) patents were categorized as having: radicular pain or radiculopathy (i.e. unilateral pain, SLR test positive, MRI finding of foraminal or lateral stenosis); neurogenic claudication (i.e. bilateral pain, SLR test negative, MRI finding of significant central canal stenosis); or a combination of radiculopathy and neurogenic claudication (i.e. bilateral or unilateral pain with MRI finding of significant central canal and lateral/foraminal stenosis) as the cause of leg pain and reduced ST and WT (Kalichman and Hunter, 2008). Based on DP determined using the MDT® system, patients were categorized as having no DP, DP with extension principle, DP with extension and lateral principle, DP with flexion principle, DP with flexion and lateral principle, and DP with lateral principle (McKenzie and May, 2003). Directional preference was confirmed by the treating physiotherapist within the first three treatment sessions.
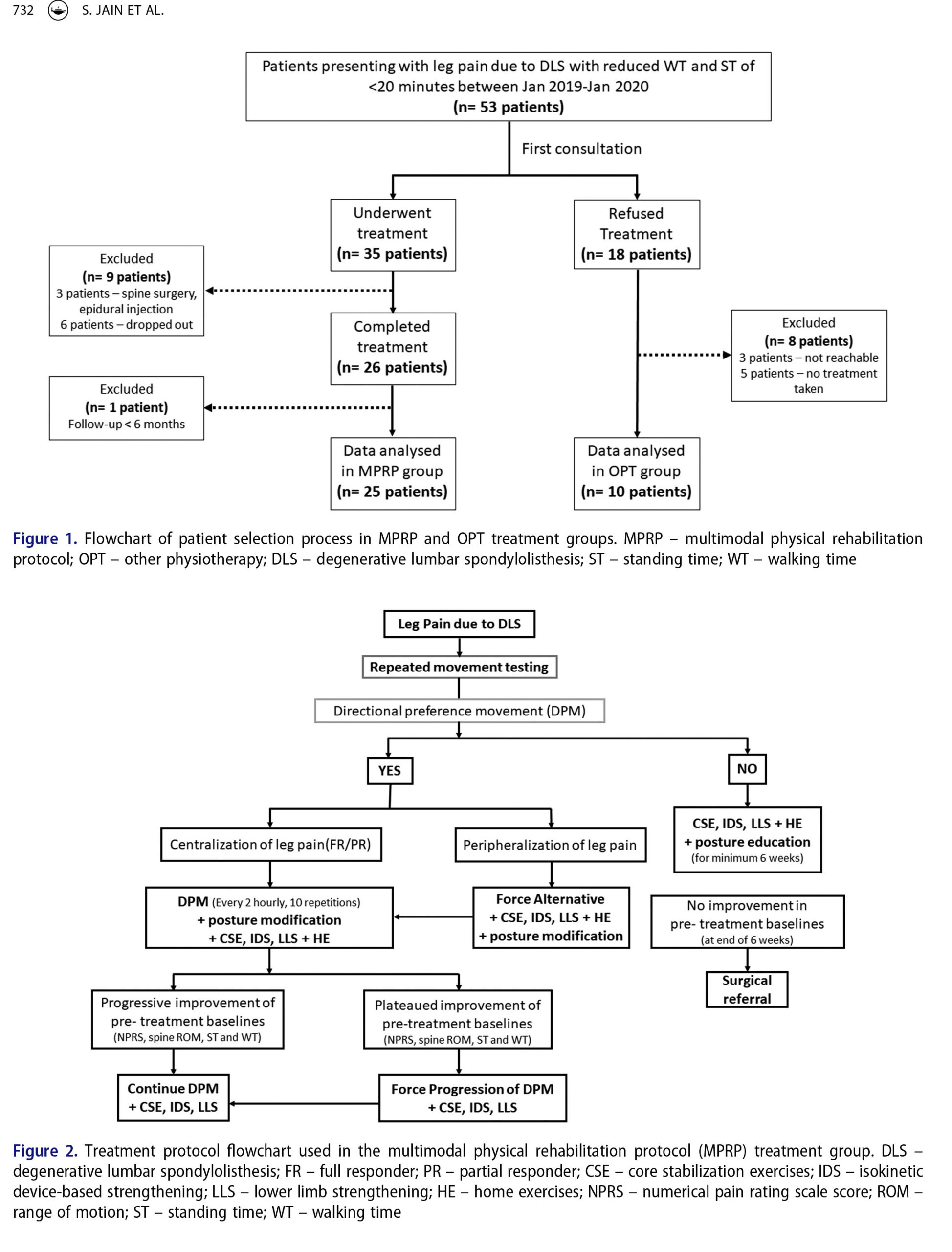
A multimodal physical rehabilitation protocol (MPRP) using a combination of patient education, directional preference movement based on MDT® principles (McKenzie and May, 2003), isokinetic device-based strengthening exercises, core stabilization exercises, and lower limb strengthening exercises was used in all patients at the outpatient rehabilitation clinic (Figure 2). All patients received a minimum of 6 weeks of MPRP with supervised 2–3 visits of 45 minutes per week at clinic along with home exercise program. Education about maintaining proper posture and rest (breaking posture and going to a non-loading position like lying supine) when required during ADL at home or at work was given to all patients.
Repeated end range movement testing was done in all patients with leg pain due to DLS. Once directional preference movement (DPM) was confirmed by treating physiotherapist within first three treatment sessions, DPM was performed by patients at outpatient clinic under the supervision of the treating physiotherapist and were advised to continue at home at least 10 repetitions every 2 hourly (Table 1). Improvement with DPM might take the form of change in distribution of lower extremity symptoms (peripheral symptoms are reduced and centralized toward the spine), change in leg pain intensity or frequency, improved spine ROM and improved ST and WT. Patients were educated on the concept of “peripheralization” of symptoms (i.e. symptoms migrating away from the middle line of the body and toward the lower limb) and asked to discontinue any movement which caused peripheralization of pain and consult their physiotherapist for further advise (McKenzie and May, 2003). Patients were also advised on posture modification where they were asked to avoid activities which involved postures which provoked pain or may cause peripheralization (e.g. patients who had DP with extension principle were advised to avoid activities and postures which involved flexion of the lumbar spine). Patients were simultaneously started on core stabilization exercises, and lower limb strengthening exercises and its intensity was gradually increased as tolerated.
Once the pain on NPRS score was <4, paraspinal muscle strength and lumbar spine mobility was assessed using a dynamometer-based device (David Spine Concept System, David Health Solutions, Helsinki, Finland) which objectively measured lumbar spine movement loss and flexibility and paraspinal muscle strength (Anandani et al., 2015). All patients were tested on three separate testing devices specific for extension, flexion, and rotation. Testing was performed in the seated-position with the patient fastened in position with a knee-lock system and a thigh restraining belt which helped immobilize both hips and thighs and allowed the patient to move only the lower back and trunk. The position of patient on each of the three devices (extension, flexion, and rotation) during testing is shown in Figure 3. Good to excellent precision and inter and intra-operator reliability (inter/intra-observer correlation coefficient: 0.78– 0.98) for measuring maximum isometric trunk muscle strength using similar dynamometer-based isokinetic devices has been reported previously in asymptomatic subjects and in subjects with LBP (Kienbacher et al., 2014; Verbrugghe et al., 2019). The patients were then put on a customized device-based strengthening exercise protocol based on the readings of the device at clinic. As home exercise program, patients were advised to perform DPM (every 2 hourly 10 reps) along with core stabilization exercises and lower limb strengthening exercises at least 2 times a day (Table 1). Basic core stabilization exercises were started first which were gradually progressed to intermediate exercises (Table 1) based on patient’s pain level and tolerance. Similarly, lower limb strengthening exercises for muscles around the hip and knee joints were included (Table 1). Once the improvement of pre-treatment baselines like NPRS, Spine ROM, ST, WT reached a phase of plateau, force progression of DPM was done till they showed further improvement (Figure 2). In patients where repeated end range movement testing produced peripheralization, force alternative movement was applied according to MDT® principles till partial or full response was elicited (Figure 2). In patients where no DP was available, posture education, customized device-based strengthening exercise (if NPRS <4), core stabilization exercises, and lower limb strengthening exercises were started and continued for at least 6 weeks with supervised 2–3 visits of 45 minutes per week at clinic along with home exercise program (Figure 2). All patients were advised to continue home exercise program at least once a day to maintain improved clinical outcomes after discharge.
Subjects in the OPT group, who refused treatment at our rehabilitation clinic and took treatment elsewhere, underwent other methods of conservative treatment under another physiotherapist which included device based thermal massaging (CERAGEM Master V3 Thermal Massage Bed, CERAGEM International Inc., Los Angeles, USA) with trunk strengthening exercises (1 patient), standard strengthening exercises for the lumbar spine with or without non-steroidal anti-inflammatory drugs (NSAIDs) (five patients), electrophysical modalities (short wave diathermy and interferential current) and lumbar strengthening exercises (three patients), and yoga (one patient). The treatment method in the OPT group was not standardized and varied depending on the treating physiotherapist’s technique. Patients underwent treatment sessions typically lasting for 30–40 minutes per sessions, 2–3 times a week with a total treatment duration of 6–12 weeks of treatment based on the type of treatment modality used and included home exercise program for strengthening exercises.
Data used in this study was obtained from patient history, examination, X-rays, MRI, and patient questionnaires completed at baseline (during first consultation). Pre-treatment pain intensity was measured using the numerical pain rating scale (NPRS) with pain intensity ranging from “0” (no pain) to “10” (worst pain imaginable) (Childs, Piva, and Fritz, 2005); and functional disability was recorded using the Oswestry disability index (ODI) score (Fairbank and Pynsent, 2000). For measuring the standing time (ST) and walking time (WT), a modification of the self-paced walking test (SPWT) which measured walking time was used (Tew et al., 2013). ST was measured using a self-reported maximum standing time method where the maximum time (in minutes) a patient can stand on a flat surface before leg pain forces them to sit was recorded using a phone based timer; and WT was measured using a selfreported maximum walking time method where the maximum time in minutes a patient can walk at their usual pace on a flat surface before leg pain forces them to stop was recorded using a phone based timer. Outcome measures were recorded in both groups by physiotherapists from the clinic who were unaware of the purpose of this study. Outcome variables in the MPRP group were recorded in clinic at three time points: (1) 4 weeks posttreatment; (2) discharge; and (3) maximum or final follow-up. Subjects in the OPT group were telephonically contacted and their treatment details and outcome variables (NPRS score, ST, WT) were recorded at two time points: (1) 4 weeks from date of first consultation; and (2) maximum or final follow-up.
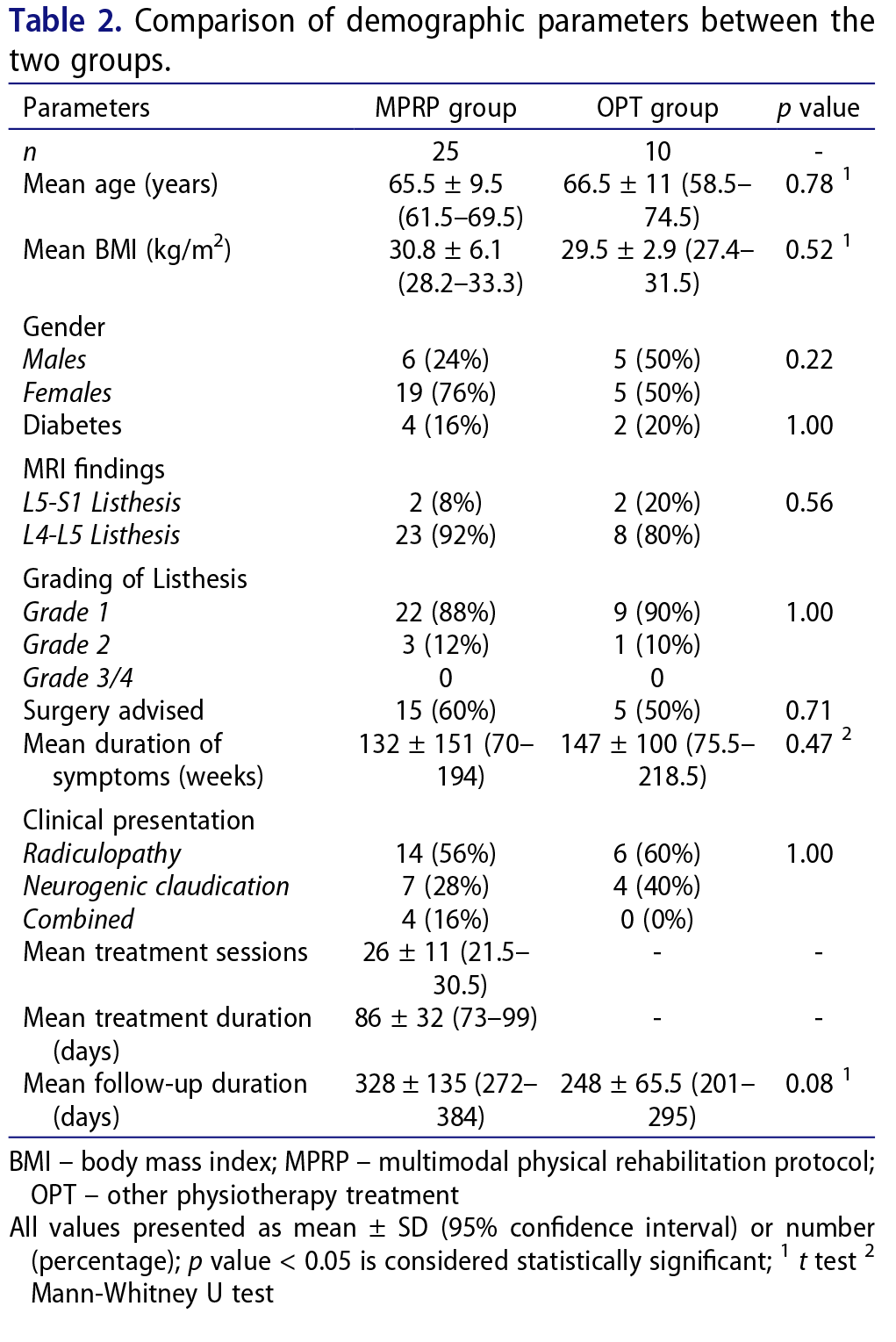
A sample size calculation using walking time as the primary outcome variable, type-I error (alpha) set at 0.05, the power set at 0.8, a minimum mean difference in walking time between the two groups at 15 minutes, and a 2.5 enrollment ratio revealed a minimum sample size of 19 patients in the MPRP group and 7 patients in the OPT group. The minimum post-treatment mean difference in walking time was set at 15 minutes based on a previous study performed in subjects with neurogenic claudication due to lumbar spinal stenosis who reported significant improvement in walking time and a mean walking time improvement of 11.1 minutes (95% CI 4.2–18.1 minutes) after treatment (Rainville et al., 2012). Demographic data including gender, age, body mass index (BMI), history of diabetes, osteoporosis, smoking and night pain, X-ray and MRI findings, directional preference on MDT® assessment, treatment sessions done and total treatment period were analyzed in the study group. Pre-treatment clinical outcome variables of NPRS score, ODI score, ST and WT were compared with values at 4 weeks of treatment, at discharge, and at final follow up. The normal distribution of sample was determined for different variables using the Shapiro Wilk (SW) test. Based on SW test, ST, WT, improvement in ST and WT, and mean duration of symptoms had non-normal distribution (SW test p < .05), whereas age, BMI, follow-up duration, NPRS and ODI scores, and improvement in NPRS score had normal distribution. Continuous data with non-normal distribution were compared using the Mann-Whitney U test whereas continuous data with normal distribution were compared using the t test or Chi square test. Categorical data were compared using the Fisher’s test.
A multivariate analysis was performed to determine the effect of pre-treatment variables such as age, gender, symptom duration, pre-treatment ST, pre-treatment WT, pre-treatment NPRS and ODI scores and treatment group on NPRS score, ST and WT at final follow. A p value of < 0.05 was considered significant. Statistical analysis was performed using the GraphPad QuickCalcs online statistical analysis tool (GraphPad Software, San Diego USA).
Of the 53 patients eligible for the study based on the inclusion criteria, 35 patients (66%) enrolled to start treatment at our clinic and were part of the MPRP group and 18 patients (34%) who refused treatment at our clinic became part of the OPT group. The reasons for a patient’s refusal to take treatment included inability to visit clinic for supervised treatment sessions due to distance or lack of time, treatment cost, and inability or unwillingness to undergo the full prescribed treatment. Two patients who underwent spine surgery, one patient who took an epidural corticosteroid injection (8.5%), and 6 patients who did not complete their prescribed treatment (17%) were excluded from the MPRP group. Due to inadequate follow-up (<6 months), 1 out of 26 patients (4%) who underwent complete treatment in the MPRP group was excluded. In the OPT group, 3 out of 18 patients (17%) who were not contactable at final follow up, and 5 patients who did not undergo any specific PT treatment for their condition were excluded. Hence, based on the exclusion criteria, data from 25 patients in the MPRP group and 10 patients in the OPT group were analyzed (Figure 1).
The baseline demographic parameters in both groups are summarized in Table 2. There were no significant differences between the 2 groups in terms of age, gender, BMI, presentation, duration of symptoms, and radiographic findings (Table 2). Out of 25 patients in the MPRP group, 21 patients (84%) had both back and leg pain, and 4 patients (16%) had only leg pain. The clinical presentation was radiculopathy in 56% of patients, neurogenic claudication in 28% of patients and combination in 16% of patients. Based on MDT® categories for DP, 56% patients had DP based on extension principle, 16% patients had no DP, 12% patients had DP based on flexion principle with lateral component, and 8% patients had DP based on flexion principle and lateral principle each. The distribution of directional preference in patients based on leg pain subgroups is shown in Figure 4. A significantly higher percentage of patients with radiculopathy showed DP with extension when compared to patients with neurogenic claudication (p = .0001) whereas a significantly
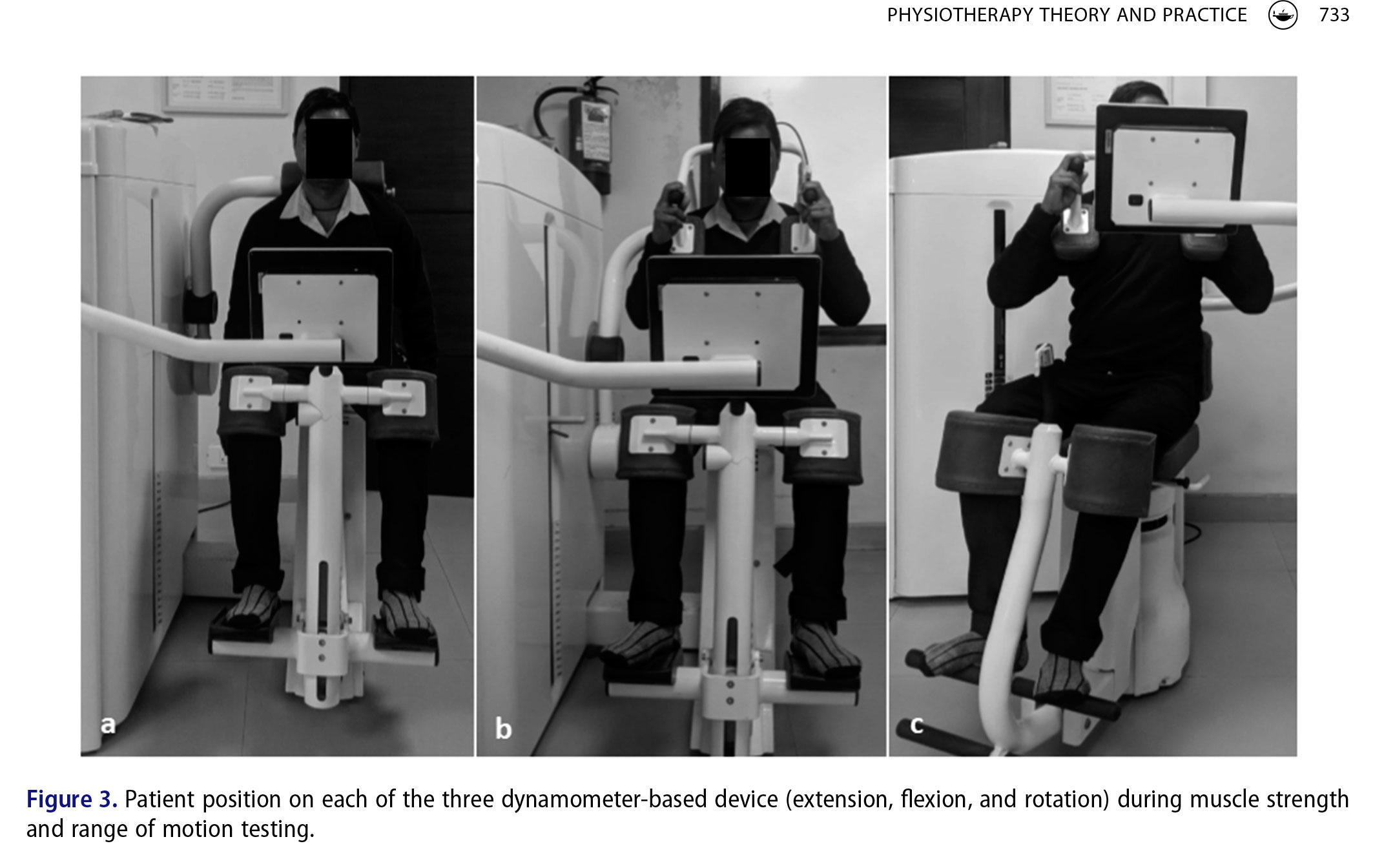
higher percentage of patients with neurogenic claudication showed DP with flexion or flexion with lateral component when compared to patients with radiculopathy (p = .0001) (Figure 3). No adverse events were found during treatment or follow-up among patients in either group.
In the MPRP group, the mean pre-treatment NPRS score of 7.2 ± 1.3 significantly reduced (p < .0001) to 4.1 ± 1.4 at 4 weeks post-treatment, significantly reduced (p < .0001) to 1.8 ± 1.1 at discharge, and significantly reduced (p < .0001) to 1.2 ± 0.8 at maximum or final follow-up. Similarly, the mean pre-treatment ODI score of 59.3 ± 9.4 significantly reduced (p < .0001) to 37.3 ± 9.2 at 4 weeks post-treatment, significantly reduced (p < .0001) to 23.5 ± 7.6 at discharge, and significantly reduced (p < .0001) to 22.5 ± 7.8 at maximum or final follow-up.
The mean pre-treatment ST of 5 ± 2.7 minutes significantly increased (p < .0001) to 13.2 ± 5.1 minutes at 4 weeks post-treatment, significantly increased (p < .0001) to 25 ± 12.5 minutes at discharge, and significantly increased (p < .0001) to 28.6 ± 13.2 minutes at maximum or final followup. Similarly, the mean pre-treatment WT of 6 ± 3.6 minutes significantly increased (p < .0001) to 13.6 ± 4.3 minutes at 4 weeks post-treatment, significantly increased (p < .0001) to 25.4 ± 12.9 minutes at discharge, and significantly increased (p < .0001) to 27.2 ± 12.1 minutes at maximum or final follow-up. None of the patients underwent spine surgery or epidural injection at final followup.
In the OPT group, the mean pre-treatment NPRS score of 5.9 ± 2.2 was not significantly different when compared to mean NPRS score of 4.9 ± 2.9 at 4 weeks from date of first consultation (p = .39), and to mean NPRS score of 4.0 ± 3.0 at maximum or final follow-up (p = .12). The mean pre-treatment ST of 9.9 ± 6.2 minutes was not significantly different when compared to mean ST of 13.3 ± 7.9 minutes at 4 weeks from date of first consultation (p = .29), and to mean ST of 18.0 ± 10.8 minutes at maximum or final follow-up (p = .05). Similarly, the mean pre-treatment WT of 10.1 ± 6.0 minutes was not significantly different when compared to mean WT of 13.8 ± 7.2 minutes at 4 weeks from date of first consultation (p = .22), and to mean WT of 18.5 ± 11.5 minutes at maximum or final follow-up (p = .05).
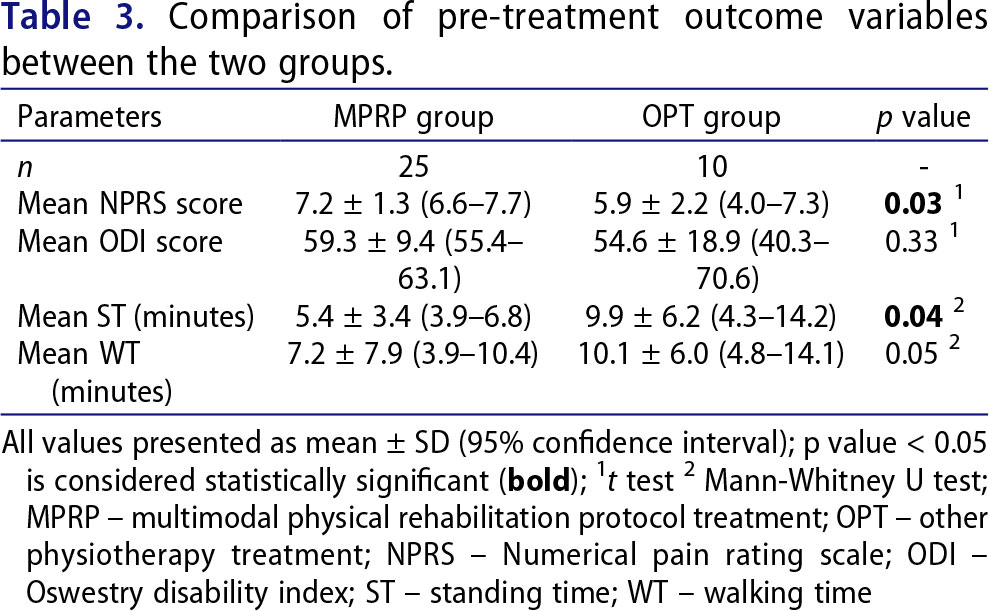
Pre-treatment, the mean NPRS score was significantly higher and the mean ST was significantly lower in the MPRP group, whereas the mean ODI score and mean
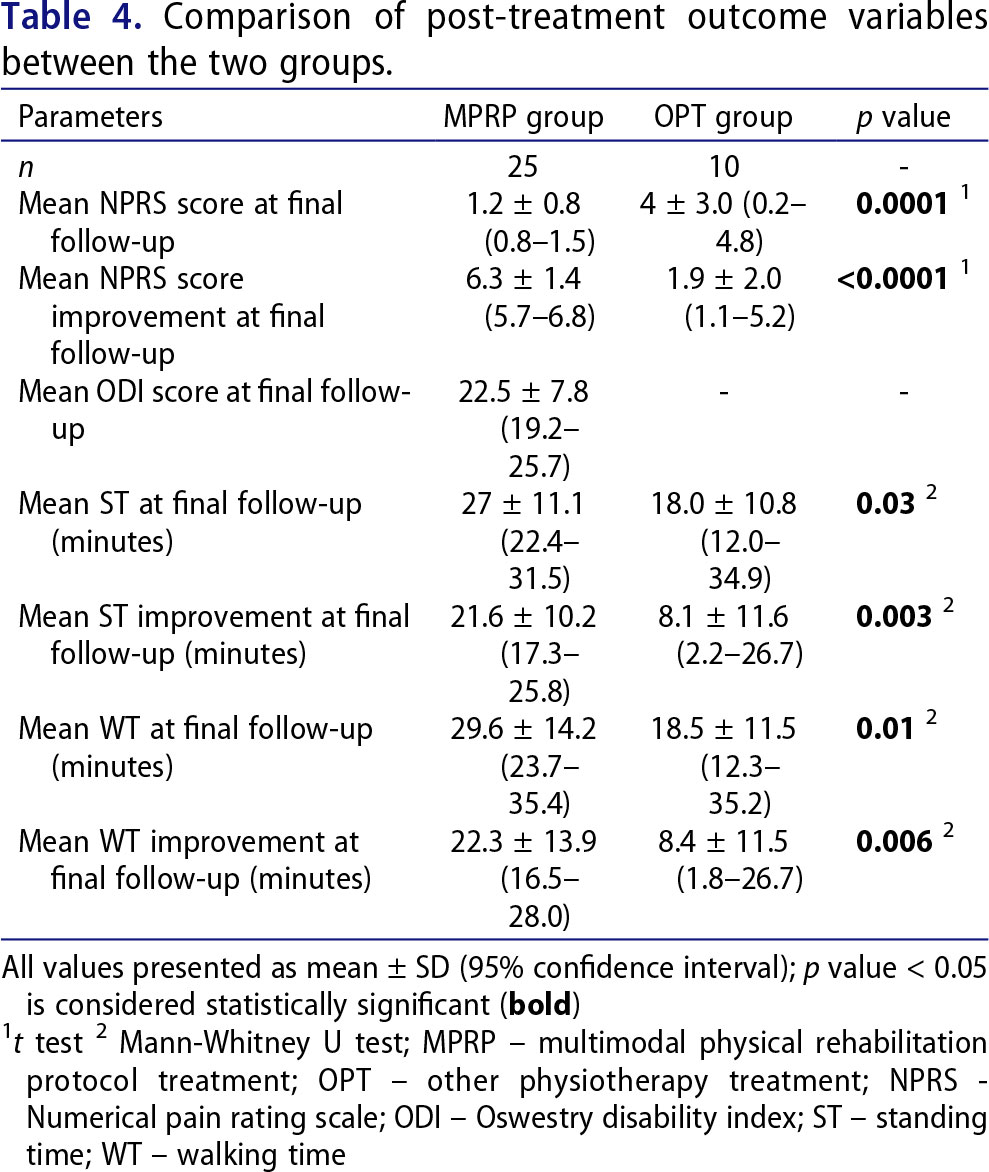
WT were not significantly different when the 2 groups were compared (Table 3). At 4 weeks, the mean NPRS score (p = .27), the mean ST (p = .96), and the mean WT (p = .91) were not significantly different when the two groups were compared. However, the mean NPRS score was significantly lower in the MPRP group whereas the mean ST, WT, and the mean NPRS, ST, WT improvements were significantly higher in the MPRP group when compared to the OPT group at final follow-up (Table 4). None of the patients in both groups underwent spine surgery or epidural injection at final follow-up.
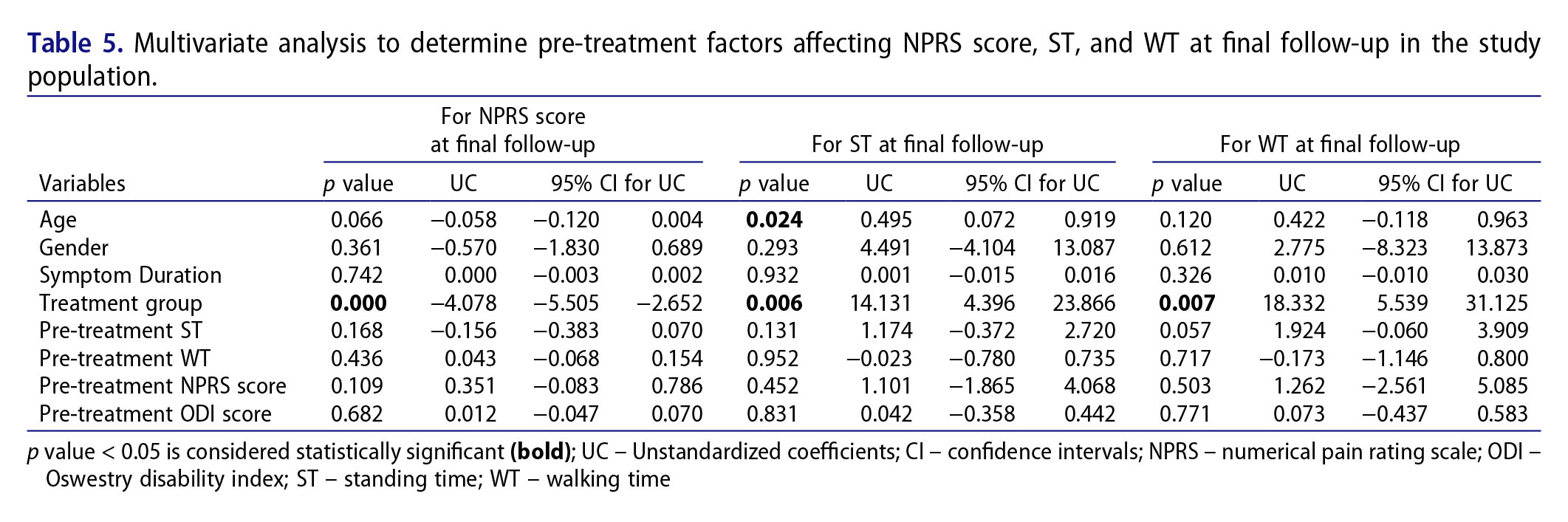
Based on the results of multivariate analysis, MPRP treatment was associated with lower NPRS score, higher age and MPRP treatment were associated with higher ST, and MPRP treatment was associated with higher WT at maximum or final follow-up (Table 5).
The findings of our study indicate that clinical outcome parameters of NPRS score, ODI score standing time and walking time can improve significantly in patients with low grade DLS treated with MPRP. Furthermore, the ST and WT in the MPRP group showed significant improvement at a mean follow-up of 328 days when compared to pre-treatment values, indicating longer term effect of the MPRP treatment. The ST, WT, and the mean improvement in NPRS score, ST and WT were significantly higher in the MPRP group when compared to the OPT group at final follow-up. Non-operative treatment has been recommended for DLS and has shown encouraging results in low grade DLS patients (Evans and McCarthy, 2018; Hardwick et al., 2012; Matsunaga, Ijiri, and Hayashi, 2000; Matz et al., 2016; Pearson et al., 2008). Pearson et al. (2008) in an analysis of radiographic predictors of clinical outcomes after operative or non-operative treatment of DS reported that non-operative treatment achieved better outcomes if patients with DS had a grade I listhesis when compared to grade II listhesis. Matsunaga, Ijiri, and Hayashi (2000) in a long-term follow-up study of non-surgically managed patients with degenerative spondylolisthesis (DS) reported that conservative treatment consisting of bracing, NSAIDs, and/or lumbar exercises is useful for patients who have low-back pain with or without pain in the lower extremities. Furthermore, 76% of patients in their study who had no neurological deficits at initial examination remained without neurological deficit after 10 years of follow up whereas 83% patients who had neurological symptoms at initial examination and refused surgery experienced neurological deterioration. However, previous studies reported clinical outcomes in terms of pain, general disability using ODI scores and change in neurological status of patients undergoing non-surgical conservative management of low grade DLS (Matsunaga, Ijiri, and Hayashi, 2000; Pearson et al., 2008). In contrast, the current study reported clinical outcomes in terms of improvement in ST and WT, a major cause of functional disability in patients with low grade DLS, treated with non-pharmacological, rehabilitative management. Based on multivariate analysis, MPRP treatment and greater pre-treatment standing time were associated with lower NPRS score at final follow-up; higher age and MPRP treatment were associated with better ST; and MPRP treatment was associated with better WT at final followup (Table 5) indicating that MPRP intervention is a significant factor determining NPRS, ST, and WT at final follow-up.
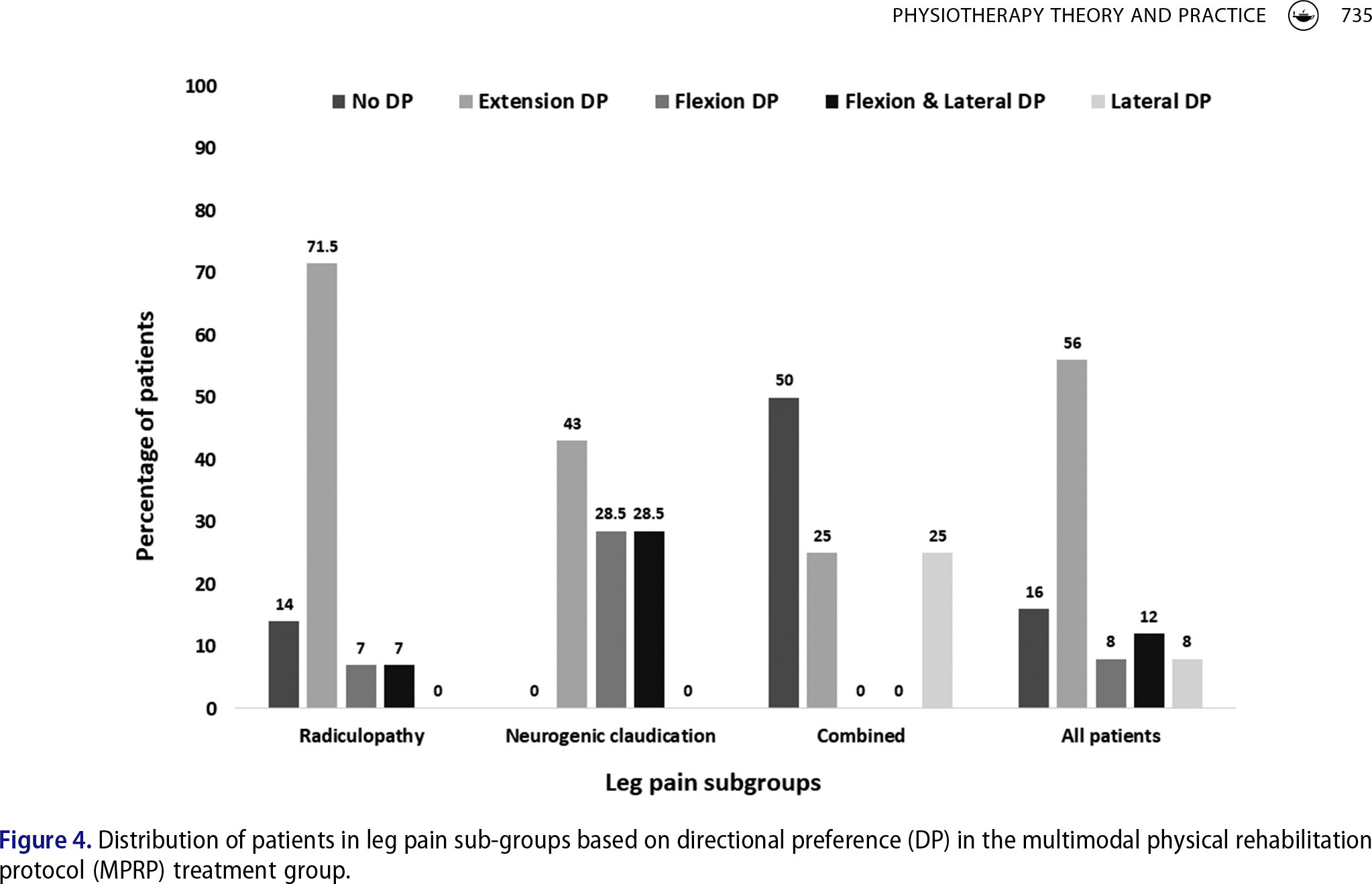
Although physical rehabilitation exercises with or without bracing, NSAIDs and epidural steroid injections have been used in patients with DLS (Bydon, Alvi, and Goyal, 2019) the type of physical therapy most effective in improving clinical outcomes is unclear. Flexion-based exercises have been reported to achieve better pain relief and functional improvement when compared with extension-based exercises (Garet, Reiman, Mathers, and Sylvain, 2013; Gramse, Sinaki, and Ilstrup, 1980; Sinaki et al., 1989). However, in the current study, 56% of all patients, 71.5% of patients with radiculopathy and 43% of patients with neurogenic claudication had a response with extension movements whereas 8% of all patients, 7% of patients with radiculopathy and 28.5% patients with neurogenic claudication had a response with flexion movements (Figure 3). This indicates that
There are some limitations to this study. First, the cause of leg pain in patients with DLS in the MPRP group was categorized as secondary to radiculopathy, neurogenic claudication or mixed type based on clinical presentation and MRI finding. This has not been investigated previously in the literature and was based on the authors’ observation and similar mention in the literature (Kalichman and Hunter, 2008). Since the aim of the current study was to investigate the effect of a multimodal physical rehabilitation protocol (MPRP) on walking and standing time in patients with DLS, this categorization of leg pain in patients with DLS needs further validation through a separate study. Second, the design and methodology of this study may have introduced biases and the reader should interpret these results with caution. Patients in the OPT group were telephonically assessed during final follow-up to record ST, WT, and NPRS score due to logistic and economic reasons whereas patients in MPRP group were assessed in person. This may have introduced a measurement bias leading to imprecision impacting the results of this study. However, previous studies have reported the validity of self-reported patient estimated maximum walking distance (Frans et al., 2019; Tew et al., 2013). Similarly, patients in this comparative study were not randomized to MPRP or OPT treatment groups and the choice of undergoing MPRP treatment at the clinic was left to patients during the first consultation which may have introduced selection bias in this study. Subjects in both groups, physiotherapists from our clinic who recorded the outcome variables at discharge and final follow-up in both the groups, and physiotherapists who treated patients in the OPT group elsewhere were unaware of the purpose of this comparative study which may have diminished the risk of observer and performance biases. Although both groups were similar in terms of baseline variables and a multivariate analysis confirmed the significant effect of only treatment mode (MPRP or OPT) on post-treatment outcome, several baseline characteristics in both groups such as comorbidities, psychosocial factors, and deviations from intended intervention, especially in the OPT group, were not included in this analysis and may have introduced a confounding bias. Third, variations in treatment time, lack of details of activity selection and exercise specificity within the control group may have impacted the results within this heterogenic group and makes replication of this study challenging. Hence, the findings of this pilot study needs to be further confirmed with a randomized controlled trial (RCT) comparing MPRP and other PT methods used in the treatment of DS.
Multimodal physical rehabilitation treatment can help significantly improve ST and WT in the short-term in patients with low grade DLS when compared to similar patients who underwent other physiotherapy treatments. However, in view of methodological limitations of the current study, the reader should exercise caution when interpreting or applying these results in the clinic.
Disclosure statementThe authors report no declarations of interest.
FundingThe author(s) reported there is no funding associated with the work featured in this article.
ORCIDShikha Jain MPT http://orcid.org/0000-0002-5905-7584 Sanya Linjhara MPT http://orcid.org/0000-0002-3181- 6534 Abhay Nene MBSS, MSOrth http://orcid.org/0000-0001- 7882-3611 CS Ram MSPT, MCA http://orcid.org/0000-0002-4576- 4544
Visit our nearest clinic for your first consultation