Request Appointment
Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.

Intense pain felt aroun the hips and the pelvis

Pelvic girdle pain (PGP) describes lower back and/or pelvic pain that stems from the ligaments and joints running from your spine to your pelvis. These include the sacroiliac joint, the pubic joint, and ligaments. Although PGP is most often discussed in the context of pregnancy, sometimes called pregnancy-related pelvic pain, it can also arise after trauma, from degenerative changes, or following surgery.
According to the patients with PGP, it is a sharp, nagging pain in the front, rear, or side of the pelvis. This pain may be worse when standing on one leg, climbing stairs, or rolling over in bed. As an integral part of the structure, and due to the presence of the spine, the alteration in the position of the said ‘girdle’ can cause certain stress and therefore disorder on the lower back and hips.
Recognition of the pain early is simply possible when you understand the symptoms, and the diagnosis enables targeted pelvic girdle pain treatment. Focusing on gentle pelvic stabilization exercises to restore joint alignment and muscle balance. In more severe conditions, extra stabilizations, namely, belts used around the pelvic region, may be of much assistance to the patient until the situation improves.
20% of pregnant women experience pelvic girdle pain from late pregnancy onwards. The pain affects the front of their pelvis, lower back, inner thigh, abdomen, buttocks, and vagina. 5-8% of women suffer from severe pain, and it affects their mobility.
Pelvic girdle pain intensifies during labour and lasts between late pregnancy and post-birth. The symptoms are:
Effective pelvic girdle pain relief therapy combines manual techniques, targeted strengthening, and posture education. Integrating pain management for pelvic girdle structures and patient‑specific exercise regimens helps restore stability, reduce pain, and improve function over time.
Pregnancy is usually a normal process, but some symptoms must be reported to the doctor of a pregnant woman. Even if you’re receiving pelvic girdle pain treatment or managing pregnancy-related pelvic pain, these warning signs should not be ignored:
Any form of red coloured loss during the rest of the pregnancy may be a sign, such as placental abruption or placenta previa. Although the pain may hardly be noticeable, one should seek medical attention immediately.
Severe head and vision problems could indicate preeclampsia or elevated blood pressure and pressure on some of the vital organs.
Sudden or persistent pain in the lower abdomen or low pelvic pain may denote features of a tear in the Uterus, preterm labor, or pain caused by round ligament strain.
An adult's body temperature above 100.4°F (38°C), accompanied by chills or extreme tiredness, would mean the patient is infected. Proper treatment is imperative to avoid complications such as Sepsis or Preterm labour.
Any decrease in the frequency of a baby’s movements, let alone a complete absence of movements after 28 weeks, should be reported to a health care provider.
This is because if any of these symptoms are felt, it is advised to consult with the doctor or visit the emergency center. It is important to detect it in the early stages to increase the chances of good health for both you and your baby.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyPelvic girdle pain (PGP) involves several interrelated structures during pregnancy that can cause the pain. Understanding these causes helps guide targeted pelvic girdle pain therapy and effective PGP management.
During pregnancy, a woman’s body produces high amounts of a hormone called relaxin that causes the ligaments in the pelvis to relax. This again helps the birth process, but weakens the joint for overall stability, and the girdle bones may easily experience slight pain.
Emotional stress on the body leads to high tension on the muscles and physical workload, likely to reduce the strength of the muscles that are responsible for pelvic support. Over time, this combination exacerbates discomfort and may delay recovery without proper pelvic pain relief strategies.
Pregnancy changes start when the fetus starts growing within the uterus, causing the mother’s center of gravity to shift forward, which puts a mechanical stress on the pelvis. The added pressure can irritate pelvic joints and surrounding soft tissues, often requiring pelvic girdle pain therapy that includes pelvic stabilization exercises.
Pain deep in the lower abdomen causes during weight-bearing movements is characteristic of the sacroiliac joint or pubic symphysis, also known as girdle pain. Adequate pelvic support therapy, such as belts or manual techniques, can help reduce joint irritation.
PGP is much more frequent in people who have had earlier spinal problems in their lumbar/sacral region. Initial propensity to have backache will affect movement and loading patterns that can, in turn, stress the pubic joints, hence requiring multiple interventions on the back and pubic joints.
It is apparent that pelvic girdle pain partly results from changes in hormones, mechanical pressure, and previous problems with the musculoskeletal system. A tailored approach, combining physical therapy for pelvic pain, hip pain treatment, and personalized pelvic girdle pain therapy, can restore stability, reduce pain, and improve functional mobility.
The causes for pelvic girdle pain are unclear, but it usually involves a history of lower back pain or having experienced pelvic girdle pain in a previous pregnancy. Other factors are:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyPelvic Girdle Pain (PGP) treatment involves upper and lower extremity mobility, controlling self-care measures, and physical therapy techniques. The following is the list of possible treatments:
Some possible measures might include avoiding daily activities that cause pain, for example, climbing stairs or reaching, and using appropriate chairs that do not harm the back support, such as lumbar support.
Some of the lower approaches include gentle stimulation of the deep core and pelvic floor, helping to improve SI joint stability. Exercises like pelvic tilts, heel slides, and “drawing‑in” maneuvers form the cornerstone of pelvic stabilization exercises.
A qualified physiotherapist needs to formulate a plan that may involve mobilization, or guided progressive strength training, and other techniques that may align the body and its movements.
Maternity belts or pelvic support bands are devices that come to the aid of the body by applying forces outside the muscles and joints to combat joint looseness. They are especially useful during walking or standing in that they recycle and augment the energy that has been expended.
Applying forces to the ligaments of the pelvis through skilled soft-tissue mobilization and joint mobilization will assist with breaking down tension throughout the muscle and pump out the stagnant fluids around the ligaments.
In cases where needed, paracetamol or pregnancy-appropriate NSAIDs can be taken for short-term use only. Alternatively, heat or cold pack box drivers may also be applied directly to painful locations.
Avoiding flare-ups entails learning proper mechanics of motion that includes movement such as turning from the hips rather than leaning from the waist. While at work, ergonomic advice helps to get the sitting and rising position right, the correct ways of lifting objects, and the right position of the spine when sitting or working.
Frequency-specific microcurrents are administered to the affected area to reduce pain and restore muscle strength. FSM therapy has been proven to enhance the healing process in damaged soft tissue and can potentially reduce inflammation. It is a safer, more effective way to reduce pain & and has no long-term side effects compared to most painkillers.
As part of a comprehensive pelvic girdle pain relief treatment approach, combining these options ensures both immediate symptom control and long‑term functional restoration. Adherence to prescribed therapies under the supervision of a qualified doctor can help increase movement considerably. If you want to speak to one of the spine doctors at QI Spine, you can use the option of our one free in-clinic or virtual consultation through a video chat.
When it comes to the management of pelvic girdle pain, it is evident that there are some practical changes as well as supportive measures that can be implemented. The following are among the ways that can be useful in the reduction of discomfort and still lead to better everyday functioning:
Try to use two feet on the stairs at once instead of placing one foot at a time on the next step, and do not lean on one leg when dressing. Sit with both feet flat on the ground and knees bent no higher than your hips. Avoid crossing your legs, as this can strain your pelvis. Small changes form part of a comprehensive pelvic girdle pain relief treatment plan.
Coordinate the movements of the transverse abdominis and pelvic floor muscles before any movement or positional change. This “bracing” technique assists in lessening the load that the sacroiliac joints take and helps in stabilizing the pelvis and the spine. Incorporating this habit into daily movements is a key component of successful pelvic girdle pain therapy.
Having a small it between the knees while sleeping can help prevent the pelvis from twisting by ensuring that it remains straight. Side-lying with knees slightly bent and hips stacked promotes lower back pain relief and lowers overnight discomfort.
An optimally fitted belt or pelvic brace is a separate and strengthens the external load-bearing points on the pelvis and shares the load more evenly. This extra pain while standing, walking, or carrying out activities such as doing house chores can be reduced by increasing stability.
Combine these self‑help techniques with a tailored program of physical therapy for pelvic pain or pelvic girdle dysfunction therapy. QI Spine’s spine therapists will teach you targeted exercises, manual techniques, and posture corrections to maximize relief and prevent flare‑ups.
By incorporating such techniques, replacing activities, reporting exercises, regulating muscles, using correct sleeping position, and using supportive structures, you can manage pelvic girdle pain and improve your functionality.
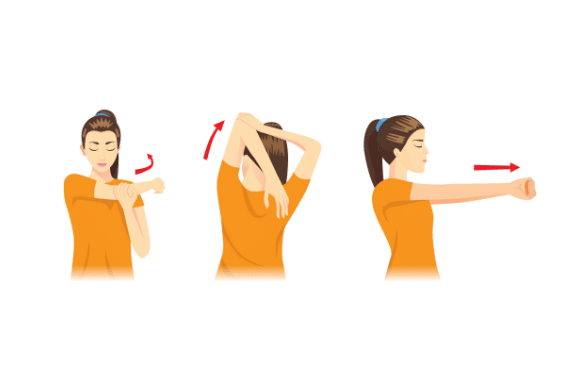
It starts from lying flat on your back with your Legs flexed at the knee joint. Get comfortable and slide your feet on the floor with your knees remaining apart; flatten your back; squeeze the glutes before you release. Sustain the contraction for 10–15 repetitions to tighten deep abdominal and pelvic floor muscles.
Lying on your back, elevate your hips toward the ceiling with a tight buttock contraction. This must be done by holding the ‘air’ for 5–10 seconds before lowering slowly. This movement stretches the muscles of the hips, but it also strengthens the hips, buttocks, as well as lower back muscles.
Progress straight on the toes of your right leg and your knees/hamstrings of the left leg, your buttocks on the ground. Each position is held for five seconds, followed by changing sides. This exercise improves the abdominal muscles and helps develop the body’s muscle equilibrium as well.
Begin on hands and knees. Expires as you move upward, extending your back and lifting your head/tailbone as if like a cow, and then draw as if retracting your abdomen and rounding your back, tuck your chin in as if like a cat. To improve spinal and pelvic mobility, it is recommended to complete between 8 and 10 cycles through the supine and prone positions.
From the kneeling position, lower your body down and sit on your heels with your legs spread apart and extend your arms towards the mat. Place your forehead to the ground and exhale, stretching some of the lower back muscles and specifically the sacroiliac region.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyMedication is not advisable for pelvic girdle pain as it might affect the unborn baby. Other treatment methods are:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyFor diagnosing any form of pelvic pain, a doctor will assess the signs and any previous medical conditions. Physical examination or some other tests may also assist in diagnosing the type of pelvic pain. Accurate diagnosis of pelvic girdle pain (PGP) is essential for effective pelvic girdle pain therapy. The assessment commonly involves a systematic approach such that:
The clinician starts the interview by asking about when the symptoms started and where they are localized, whether it is aching, stabbing, or stinging. This helps to specify those activities that increase or decrease pain, for example, walking, standing, or resting. Any obstetric history, previous pelvic injury, or surgery is documented to understand potential contributing factors in PGP management.
A thorough examination includes:
Gait analysis, single-leg stance, and other transitional activities such as rising from a chair) Identify whether the subject uses compensatory movements/includes pelvic instability. Identifying these patterns guides pelvic girdle dysfunction therapy by revealing which muscles require stabilization.
If clinical and functional tests are negative, imaging may be done:
In some situations, the injections performed under anesthetic control into the sacroiliac joint or the pubic symphysis identify the primary affected site. A positive response to the injection helps tailor targeted physical therapy for pelvic pain.
Based on the patient history, physical examination, functional observations, imaging, and diagnostic injections, it is possible to diagnose PGP and work out an individualized treatment plan. Early and precise identification of the underlying issue ensures optimal pelvic pain relief and improved functional outcomes.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine Therapy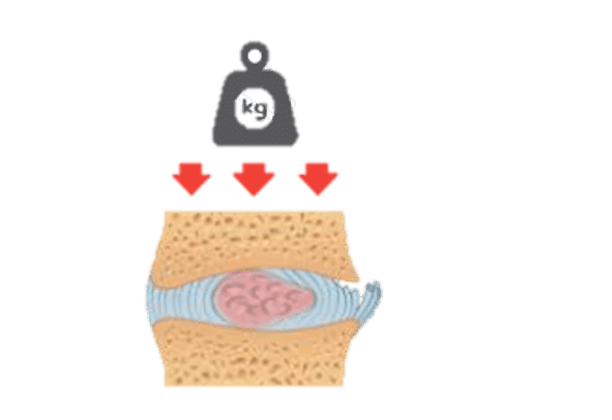

Have a question?
Ask our spine specialists
Who is a QI Spine Specialist?
A QI Spine Specialist is a medical expert with

Dr. Nidhi Sanghvi Shah

Dr. Shital Gaikwad

Dr. Richa Bhatia
9000 hours
of specialisation in treating back and neck conditions
32 hours
of spine physiotherapy specialisation methods in McKenzie concepts, Kinetic control, Neurodynamic solutions, Mulligan’s concepts
500 hours
and 6 months of QI Spine specialisation courses