Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.

inflammatory consitions affecting the spinal joints

Spondyloarthropathies are a family of chronic inflammatory disorders that primarily affect the spine and sacroiliac joints but can also involve peripheral joints, entheses (sites where ligaments attach to bone), and extra‑articular organs. Characterized by back stiffness, pain that improves with activity, and the genetic marker HLA‑B27, these conditions often emerge in early adulthood.
The immune system’s misdirected attack on joint structures leads to progressive inflammation, reduced mobility, and potential spinal fusion. Early diagnosis is vital for effective inflammatory spine disease management, and timely spondyloarthropathies relief therapy can slow disease progression and preserve function.
As Spondyloarthropathies covers a wide range of arthritic conditions that affect the joints, the symptoms will vary depending on the type of spondyloarthritis. Some of the most common symptoms associated with the condition include the following:
The prototype disorder is marked by sacroiliac inflammation and eventual vertebral fusion. Pain and stiffness are most pronounced in the morning and improve with exercise.
Associated with psoriasis, it may affect both axial and peripheral joints. Nail changes and dactylitis (“sausage fingers”) are common indicators.
Develops after certain gastrointestinal or genitourinary infections. Symptoms include asymmetric joint pain, conjunctivitis, and urethritis.
Linked to inflammatory bowel diseases (Crohn’s disease, ulcerative colitis). Joint flares often parallel bowel disease activity.
It features inflammatory back pain and peripheral arthritis without fulfilling the criteria for a specific subtype.
Management strategies encompass spondyloarthropathies therapy, from NSAIDs and biologic agents to tailored physical therapy for spondyloarthropathies to reduce inflammation, maintain mobility, and achieve long‑term chronic back pain treatment outcomes.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 8 weeks of QI Spine Therapy
Treatable with 8 weeks of QI Spine TherapyThe precise causes of spondyloarthropathies remain unknown to date, but some are associated with specific genes, such as the HLA-B27 in the case of ankylosing spondylitis. Although the gene itself is not responsible for spondyloarthritic conditions, it is associated with an increased risk.
Researchers are still investigating the relationship between genetics and the development of spondyloarthropathies. Some studies also point towards a connection between imbalances in gut flora and inflammatory disease. Reactive arthritis is the only exception since it is caused by a bacterial infection, typically involving a foodborne or chlamydia infection.
Spondyloarthropathies arise from a complex genetic, immunologic, and environmental interplay. Understanding these causes can guide early intervention and tailored spondyloarthropathies treatment approaches.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyConventional spondyloarthropathies treatments include NSAIDs (Nonsteroidal anti-inflammatory drugs) and other pain medications. The long-term use of NSAIDs is associated with stomach ulcers, an increased risk of bleeding, and liver and kidney problems. Unfortunately, there is no permanent cure for spondyloarthropathies, which means that patients are forced to take pain medications regularly to manage their pain, which significantly increases their risk of these side effects. However, QI’s holistic evidence-based treatments help to manage spondyloarthropathies with minimal to no risk of negative effects.
Conventional spondyloarthropathies therapy focuses mainly on pain medications, which only manage the symptoms of the condition but do not address the root cause of the problem. QI Spine Clinic uses some of the most technologically advanced diagnostic and treatment methods to help patients manage their condition and lead healthy, productive lives.
Over 80% of all back pain remains undiagnosed, and doctors refer to the pain as ‘unspecified’. QI Spine Clinic uses the most advanced spine function test – the Digital Spine Analysis (DSA) to pinpoint muscles and structures that have been affected by spondyloarthropathies. This allows QI spine specialists to create targeted treatment protocols to strengthen these muscles to improve muscle function, and increase mobility.
Treatment protocols are unique to each patient, depending on how the condition has affected them. This allows spine specialists to provide the best spondyloarthropathies treatment for each patient, depending on their individual requirements.
QI Spine Clinic also provides microcurrent therapy as a safe alternative to pain medication, as it does not cause any side effects. This therapy uses very low-level electrical currents to reduce muscle and nerve pain and reduce inflammation. The benefits of microcurrent therapy accrue over time, so several sessions will prove to have greater pain relief benefits. QI Spine also offers counseling and alternative therapies to help patients with spondyloarthropathies understand the physical and psychological changes associated with this condition. It is important to consult a spine specialist as soon as possible to manage spondyloarthropathies and reduce your pain.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyConventional treatments for spondyloarthropathies include NSAIDs (Nonsteroidal anti-inflammatory drugs) and other pain medications. The long term use of NSAIDs is associated with stomach ulcers, an increased risk of bleeding, and liver and kidney problems. Unfortunately, there is no permanent cure for spondyloarthropathies which means that patients are forced to take pain medications regularly to manage their pain which greatly increases their risk of these side effects. However, QI’s holistic evidence-based treatments help to manage spondyloarthropathies with minimal to no risk of negative effects.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyDiagnosing spondyloarthropathies, a group of related inflammatory rheumatic diseases, requires a systematic, multidisciplinary approach to distinguish them from other back and joint disorders.
Once confirmed, a personalized plan, including non‑steroidal anti‑inflammatory drugs and spondyloarthropathies relief treatment, such as physical rehabilitation, ensures optimal inflammatory spine disease management and long‑term chronic back pain treatment.
At QI Spine, the diagnosis is made by understanding first the patient’s history, conducting a thorough physical examination, and doing a DSA (Digital Spine Analysis test), which helps analyze the root cause of the problem. It is a non-invasive functional test that helps in measuring spine function. Its controlled and guided movements help determine the spine's mobility, strength, and imbalances of muscles around the spine.
CT scans, MRIs, and X-rays often fail to pinpoint the exact source of pain, whereas DSA directly analyzes muscle tissue to identify the root cause. Here is how DSA is conducted & its benefits:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine Therapy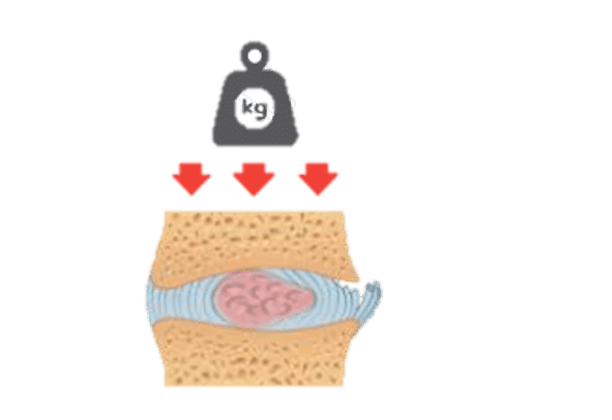

Have a question?
Ask our spine specialists
Who is a QI Spine Specialist?
A QI Spine Specialist is a medical expert with

Dr. Nidhi Sanghvi Shah

Dr. Shital Gaikwad

Dr. Richa Bhatia
9000 hours
of specialisation in treating back and neck conditions
32 hours
of spine physiotherapy specialisation methods in McKenzie concepts, Kinetic control, Neurodynamic solutions, Mulligan’s concepts
500 hours
and 6 months of QI Spine specialisation courses
Yes. Sticking to exercise, ankylosing spondylitis management, and regular health checks keeps most individuals healthy. Starting with physical therapy and the appropriate medicine can help keep muscles active and life good.
More than 90% of persistent inflammatory back pain and sacroiliac joint problems resulting from ankylosing spondylitis are caused by this.
Photos of the lower back usually show sacroiliitis, the main symptom is back pain made better with activity, and a blood test can reveal HLA‑B27 positivity, which marks spinal and entheseal involvement.
An anti-inflammatory diet high in plant foods, vegetables, fruits, lean protein, and healthy fats can aid with symptoms. Incorporating foods with anti-inflammatory characteristics, such as fatty fish, garlic, and turmeric, is also useful.