Request Appointment
Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.

Impingement of the sciatic nerve at the piriformis muscle
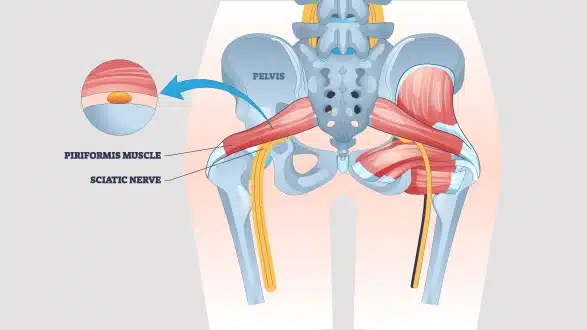
Piriformis syndrome is a neuromuscular condition in which the piriformis muscle, located deep in the buttock, irritates or compresses the sciatic nerve. The piriformis connects the sacrum to the femur and aids in hip rotation. When this muscle becomes tight, inflamed, or spasms due to prolonged sitting, overuse, or direct trauma, it can pinch the sciatic nerve, causing deep buttock pain that radiates down the back of the leg.
Symptoms typically include aching or burning discomfort in the buttock, worsened by sitting or hip movements, and may mimic sciatica but originate outside the spine. Effective piriformis syndrome therapy combines targeted piriformis stretch exercises and soft‑tissue release with activity modifications.
Incorporating sciatic nerve pain relief methods, such as heat, ice, or massage, helps reduce nerve irritation. Early recognition and a structured program of stretching, strengthening, and ergonomic adjustments restore normal muscle function and alleviate nerve compression, allowing a return to comfortable daily movement.
In a rare condition, the piriformis muscle compresses the Sciatic nerve, causing pain in the buttocks and lower limbs along the path of the Sciatic nerve.
The primary symptom is sciatica type pain in the buttocks and the legs. Additional symptoms may include:
As with many medical disorders, identifying piriformis syndrome can be complicated because various symptoms are less well-known.
The nearby nerves can get irritated, causing a sensation of radiation or numbness in the groin area. This may resemble hip joint problems or pressure on a nerve at another location.
Sometimes the affected areas are both sides of the body, and the pain felt in both buttocks and legs is symmetrical. This condition may require a broader piriformis syndrome relief therapy approach.
Muscle dysfunction, such as in the piriformis muscle, can be attributed to hormonal changes, altered body posture, and pelvic instability, which may be a result of pregnancy. In such cases, pelvic pain therapy and postpartum-specific physical interventions can help.
Some people have complaints of pain that shifts or changes in its intensity, that occurs on one side of the body first, then shifts to the other side. This is sometimes due to muscle imbalance or a change in the nerve compression point.
The mild sign is pain along and slight weakness during lateral leg movements or climbing up the stairs, or standing get-up from a sitting position.
The piriformis syndrome may present during sexual intercourse in terms of spasm or irritation of the deep and superficial muscles.
A comprehensive approach combining piriformis stretch exercises, physical therapy for piriformis syndrome, and targeted pain strategies can aid in long-term sciatic nerve pain relief and improved quality of life.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyPiriformis syndrome is a condition in which the piriformis muscle, which lies below the gluteal fold in the buttock region, affects the sciatic nerve. There are several reasons for this condition:
The most usual reason is that many leg muscles are used in activities involving such movements such as long-distance running, climbing stairs, or cycling. These activities might cause the formation of a spasm or even inflammation of the piriformis muscle that will eventually rub on the S1 nerve.
When the muscle sustains an injury, such as a fall which results in the impact on the buttocks or lower back area, the tissue may be scarred or inflamed around the said area. As a result, this may pinch the sciatic nerve and lead to regular pain or even aches.
There are cases where the sciatic nerve either runs through or bifurcates the piriformis muscle instead of through the inferolateral aspect of it. This raises the chances of nerve compression during muscle contractions or any slight movements of our body.
While there are several possibilities why the piriformis muscle gets irritated, a common cause is prolonged sitting on a hard surface. This is especially so for those who have a sedentary lifestyle, exacerbating more tension and inflammation in the muscles.
The following can be considered as the risk factors that might contribute to the occurrence of piriformis syndrome. These include:
piriformis muscle.
In such cases, piriformis syndrome relief treatment may include a combination of exercises, stretching, and therapeutic interventions.
There are specific behaviors and activities that you undertake daily, and such movements intensify or bring symptoms. Recognizing and avoiding these activities is key to better pain management for piriformis syndrome.
Incorporating piriformis syndrome exercises and guided piriformis muscle therapy can help reduce these triggers. Many individuals also benefit from piriformis syndrome therapy as part of their long-term recovery and sciatica management plan.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyPiriformis syndrome treatment focuses on reducing buttock and leg pain, stabilizing the hip and thigh, and improving mobility in the hip. Initial treatments are conservative measures such as taking 1-2 days of rest, physical therapy, and taking some medications. Injections could be given if oral medicines are not adequate in providing relief from the pain. Surgery for piriformis syndrome is only under special circumstances when the cause is significant and/or there is progressive weakness in the leg muscles.
It is common to treat piriformis syndrome patients with lifestyle changes like avoiding sitting, practicing good posture, and going for physical therapy. In mild conditions, it may be helpful to rest for 1-2 days for the symptoms to decrease. Below are the main approaches:
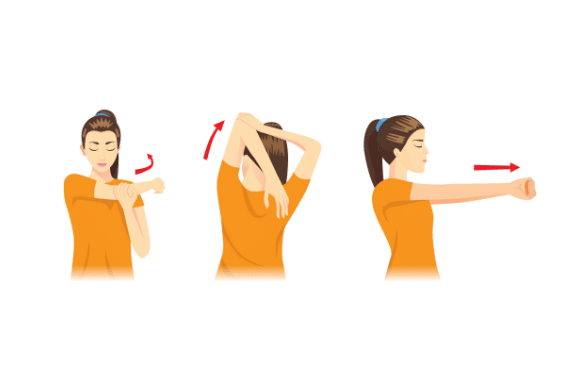
To alleviate pain resulting from a piriformis condition, recommended exercises include gentle stretching and stretching of the hip stabilizer muscles. Such routines comprise the supine piriformis stretch and clamshells for Flexibility and Support. Consistent practice of Piriformis syndrome exercises helps reduce muscle tension and improve mobility.
Common analgesics, including Ibuprofen and Naproxen, belong to the Non-steroidal anti-inflammatory drugs that help to lessen inflammation and pain. These medications provide pain management for piriformis syndrome by inhibiting the inflammatory pathways that contribute to muscle swelling and nerve irritation.
Myofascial release therapy or deep tissue massage can be incorporated as an adjuvant therapy in releasing tension in the piriformis and contributing muscles. Skilled therapists may employ trigger-point work to address localized spasms and promote piriformis muscle therapy.
Prescription muscle relaxants that are taken for a short amount of time can substantially help in relieving serious spasms in the piriformis muscles, thus enabling the patient to engage in exercises and other activities a lot more comfortably.
A particular program under a specialist involves correct posture, strengthening core muscles, and certain stretching exercises. Physical therapy for piriformis syndrome often includes manual mobilization and neuromuscular re-education to correct movement patterns that exacerbate symptoms.
Steroidal therapy administered intra-articularly to the area of the piriformis muscle will drastically reduce inflammation and offer genuine relief. It becomes helpful when other conservative interventions have not helped in managing pain.
Botox injections into the piriformis muscle interfere with the signals that cause spasms to occur, and they last several months. This technique can be an adjunct to ongoing piriformis syndrome relief treatment, especially for chronic or refractory cases.
Frequency Specific Microcurrent (FSM) is a proven pain management technology that uses extremely low frequency of electric current to treat the root cause of pain by aiding tissue repair at a cellular level. It is a safer, more effective way to reduce pain & and has no long-term side effects compared to most painkillers
Surgery is recommended only in the rarest of cases where the patient is affected by severe disability.
Targeted piriformis syndrome exercises help stretch and strengthen the piriformis muscle, relieving pressure on the sciatic nerve and improving hip mobility. Execute these movements slowly, extending the duration of the stretch to 20-30 seconds and moving through each stretch 2-3 times for each side.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyPiriformis Syndrome is treatable with conservative treatment methods, which involve
Surgery is recommended only in the rarest of cases where the patient is affected by severe disability.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyAccurate diagnosis of piriformis syndrome ensures patients receive the most effective piriformis syndrome treatment and avoid unnecessary interventions. The process followed in the diagnosis is as follows:
The clinical history for piriformis syndrome and the clinician first enquires from the patient regarding the character of the pain, which is usually a dull burning type of pain in the buttock region radiating downward to the back of the thigh, mimicking sciatica.
You should be aware of what things trigger pain, such as sitting for a long period, running, or climbing stairs, and what relieves the pain at least for some time, such as walking or standing.
Any past injury to the area, frequent movements that might compress the hip rotating muscles, or existing structural abnormalities around the sciatic nerve are elicited to observe any potential causes of nerve compression.
The practitioner abducts the patient’s leg laterally while stabilizing the trochanter just below the posterior iliac crest to check if it evoke the patient’s buttock pain and your relief is when the doctor compresses the piriformis muscle to evoke the complaint of buttock pain or modulate the patient’s pain by pressing against the ischial tuberosity on the opposite side.
Next, they evaluate the amount of pain and the range of motion in the hip’s internal and external rotations. To complement the diagnosis and determine whether the piriformis is involved, clinical tests, namely the FAIR and the Pace tests, are carried out to attempt to reproduce the discomfort felt by the patient, while seated, by flexing the hip to an angle of 60 degrees, adducting it, and then rotating it internally.
MRI/Ultrasound: Exclude lumbar disc herniation, masses, or other soft tissue sources. Imaging may show piriformis inflammation.
Bone scans: These are used when there is doubt about stress fractures or metabolic bone disease, and plain radiographs are negative.
Electro-myography/nerve conduction studies: Performed selectively where lumbar radiculopathy is suspected; if normal yet the patient’s symptoms persist, entrapment neuropathy is suspected.
An Anesthetic and corticosteroid injection into the piriformis muscle can confirm the diagnosis if it provides immediate sciatic nerve pain relief.
Rule out other conditions that may also produce buttock or leg pain, like Sacroiliac joint pain, Hamstring tendinopathy, and hip joint arthritis. Collaboration with an orthopedic specialist or physiatrist helps refine the diagnosis and plan comprehensive piriformis syndrome relief treatment.
At QI Spine, the diagnosis is done by asking about the patient’s history, conducting a thorough physical examination, and doing DSA (Digital Spine Analysis test), which helps in analyzing the root cause of the problem. It is a non-invasive functional test that helps in measuring spine function. Its controlled and guided movements help in determining the mobility of the spine, strength, and imbalances of muscles around the spine.
CT scans, MRIs, and X-rays often fail to pinpoint the exact source of pain, whereas DSA directly analyzes muscle tissue to identify the root cause. Here is how DSA is conducted & its benefits:
Detailed clinical history, tests, and diagnostic injections coupled with advanced imaging, sonoelastography, DSA, and bone scan determine piriformis syndrome. Once confirmed, a personalized plan of piriformis muscle therapy, including piriformis syndrome exercises and manual techniques, restores muscle balance, relieves nerve compression, and facilitates successful long‑term pain management for piriformis syndrome.
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine Therapy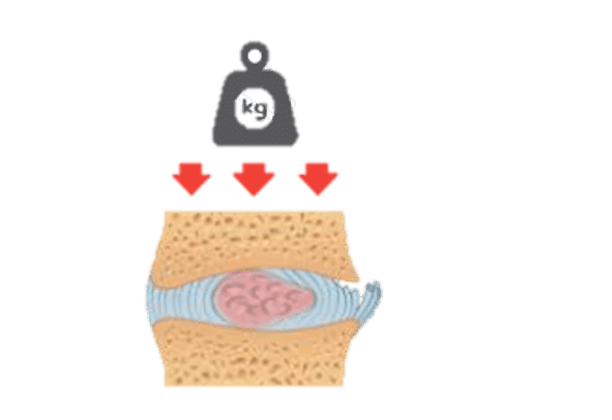

Have a question?
Ask our spine specialists
Who is a QI Spine Specialist?
A QI Spine Specialist is a medical expert with

Dr. Nidhi Sanghvi Shah

Dr. Shital Gaikwad

Dr. Richa Bhatia
9000 hours
of specialisation in treating back and neck conditions
32 hours
of spine physiotherapy specialisation methods in McKenzie concepts, Kinetic control, Neurodynamic solutions, Mulligan’s concepts
500 hours
and 6 months of QI Spine specialisation courses