Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.

A condition caused due to degeneration of the spine

Spondylosis is the most common form of spine bone degeneration that begins to affect people from middle age onwards. More than 85% of people older than age 60 are affected by spondylosis. Spondylosis is usually asymptomatic. Symptoms show up when a bone spur pinches a nerve, or simply begin with pain and stiffness.
Spondylosis is generally asymptomatic in its early stages, but as it progresses, various symptoms can emerge. To provide a clearer picture, the symptoms are discussed in two parts: Lumbar Spondylosis and Cervical Spondylosis.
Lumbar spondylosis affects the lower back and can lead to a range of symptoms that impact daily activities:
Cervical spondylosis affects the neck and the structures in that region. Its symptoms often include:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapySpondylosis is caused primarily by:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapySpondylosis cannot be cured, but milder cases can be managed with conservative treatment, which includes:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapySpondylosis cannot be cured but milder cases can be managed with conservative treatment which includes:
Advanced pain management involves:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine TherapyDiagnosing spondylosis involves a thorough and systematic approach to determine the extent of spinal degeneration and guide effective spondylosis treatment. This process helps in planning appropriate spondylosis therapy to alleviate symptoms and prevent further progression of the disease.
To diagnose spondylosis, the first thing the doctor will do is review the patient’s medical history and perform a physical examination. To understand your pain history doctor will ask questions regarding working and other activities, movements, or positions that are linked with the development of the condition. When assessing you, the following physical examination processes will be followed:
Ask the patient regarding complaints of pain in the neck and back, stiffness, and difficulty moving around. Such symptoms often warrant further investigation for conditions like degenerative disc disease and spinal osteoarthritis management.
Analysis for any signs of nerve compression, be it in the form of tingling, numbness, or weakness, as it will mean a spinal component is present.
These details are essential for planning a holistic spondylosis therapy strategy that often incorporates exercise for spondylosis and ergonomic modifications.
As a result of this, several image studies are usually done to confirm the diagnosis:
These can also be used to visualise bone spurs, joint spaces, and disc conditions to support conclusions of spinal degeneration.
MRI scans, in particular, are useful for assessing soft tissue and confirming the presence of spinal inflammation that requires non-surgical spondylosis treatment.
This is supported by the blood tests, which may be conducted to first find out whether the patient has elevated inflammatory markers and rule out other inflammatory diseases.
At QI Spine, the diagnosis is made by asking about the patient’s history, conducting a thorough physical examination, and doing a DSA (Digital Spine Analysis test), which helps analyze the root cause of the problem. It is a non-invasive functional test that helps in measuring spine function. Its controlled and guided movements help in determining the mobility of the spine, strength, and imbalances of muscles around the spine.
CT scans, MRIs, and X-rays often fail to pinpoint the exact source of pain, whereas DSA directly analyzes muscle tissue to identify the root cause. Here is how DSA is conducted & its benefits:
 Professional diagnosis required
Professional diagnosis required Chronic, can last for years
Chronic, can last for years Treatable with 4 weeks of QI Spine Therapy
Treatable with 4 weeks of QI Spine Therapy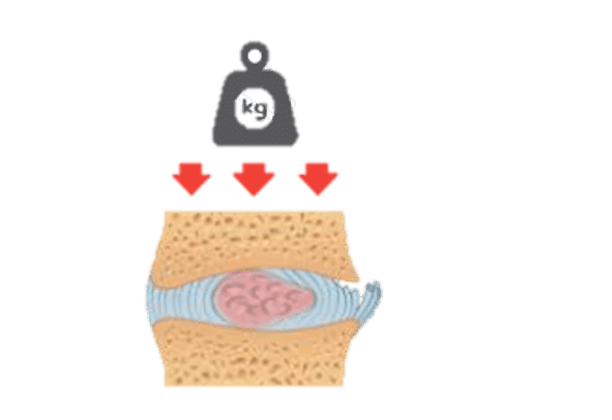

Have a question?
Ask our spine specialists
Who is a QI Spine Specialist?
A QI Spine Specialist is a medical expert with

Dr. Nidhi Sanghvi Shah

Dr. Shital Gaikwad

Dr. Richa Bhatia
9000 hours
of specialisation in treating back and neck conditions
32 hours
of spine physiotherapy specialisation methods in McKenzie concepts, Kinetic control, Neurodynamic solutions, Mulligan’s concepts
500 hours
and 6 months of QI Spine specialisation courses